Surgical Solutions Forsoft-tissue Deficienciesin Esthetic Zone:


VIP-CTG is the last resort
ABSTRACT
The esthetic zone is the most visible area of the mouth when you smile. Thus, implants in the esthetic zone pose the most challenge in cases with multiple implants or pre-existing soft tissue or hard tissue deficiencies. Given the many challenges in the esthetic zone, even the slightest deviation from the most ideal plan can lead to esthetic failure and ultimately patient dissatisfaction.
Soft tissue deficiencies are usually the main risk factor around dental implants, especially in the esthetic zone. A lack of soft tissue volume can present in many clinical situations, including attachment loss on adjacent teeth (gum recession), concavities at sites with congenitally missing teeth, and loss of interdental papillae. A significant loss of soft tissue volume can be acquired at various phases, including a loss of bone and tissue volume after tooth extractions, history of periodontal disease, history of endodontic failures or vertical root fractures, and biological implant complications.
The clinical management of these various situations may be very different, involving soft and hard tissue reconstruction with further tissue training during the temporization phase. The use of free autogenous connective tissue grafts is usually limited to smaller ridge defects due to limited donor site availability and post-operative shrinkage of the tissue (1). Pedicled autogenous grafts have been proposed to overcome the limited gain of soft tissue volume when using palatal tissue (2,3).
My article describes how to augment and correct soft tissue deficiencies in the esthetic zone using a Vascularized Interpositional Periosteal-Connective Tissue Graft (VIP-CTG) in 3 clinical situations:
- esthetic management in the case of a poorly placed implant,
- soft tissue augmentation in the case of a severe vertical and horizontal deficiency, and (3) site management in the case of congenitally missing incisors in a younger patient unsuited for dental implants due to their age.
INTRODUCTION
The periodontal and peri-implant soft tissue thickness and zone of keratinized gingiva all play an important role in a patient’s esthetic clinical appearance, the soft and hard tissue health around teeth, and more importantly dental implants, especially as we have moved away from a purely functional and survival-based implant success definition to more patient-oriented esthetically driven, natural in appearance tooth and implant restoration (4). Autogenous connective tissue grafts are still the gold standard for almost all soft tissue augmentation procedures. Connective tissue (CT) can be obtained via a free graft approach or pedicled graft approach. While free grafts are completely removed from the donor site and placed in a remote site, pedicle grafts remain attached to their blood supply and are placed immediately next to the blood supply origin (incisive vasculature or greater palatine vasculature). Retention of the blood supply has a direct positive effect on graft volume stability and less shrinkage over time. (5)
CASE 1
Management Of Poorly Positioned Implant And Gingival Recession On Natural Tooth In Esthetic Zone



A 42-year-old female patient was referred for an esthetic evaluation of a recently placed and restored implant at #9 and recession on tooth #10. The implant was very buccally positioned (by another dentist), but the patient declined removal of the newly placed implant. The decision was made to augment the soft tissue esthetics at sites #9 and 10 using a VIP-CTG.
The implant restoration at #9 and composite on tooth #10 were removed, and a cover screw was placed 3-4 days prior to soft tissue augmentation to allow soft tissue closure over the implant. This leads to a better primary closure during the surgical phase of treatment (Figure 2).


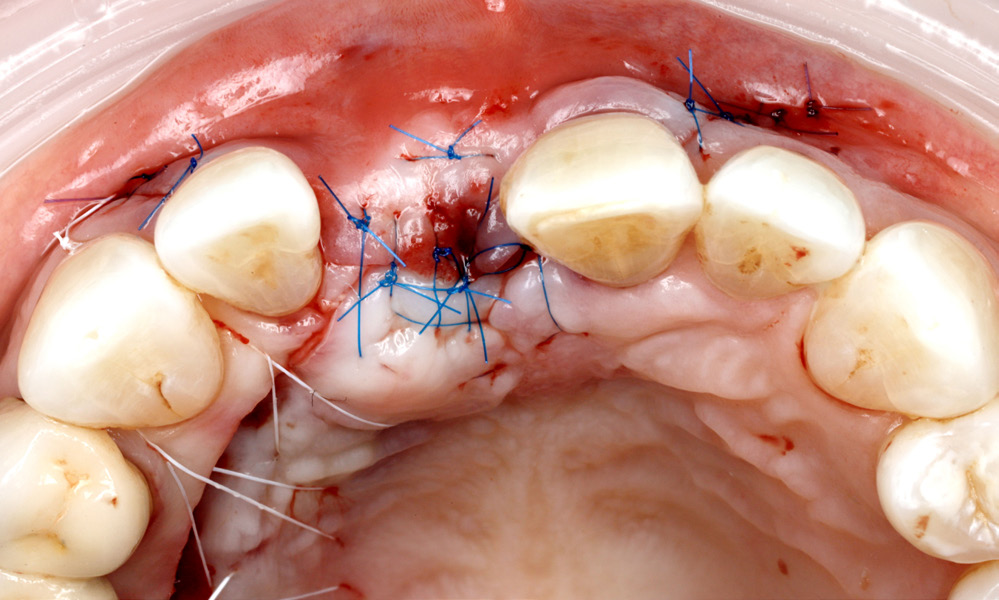
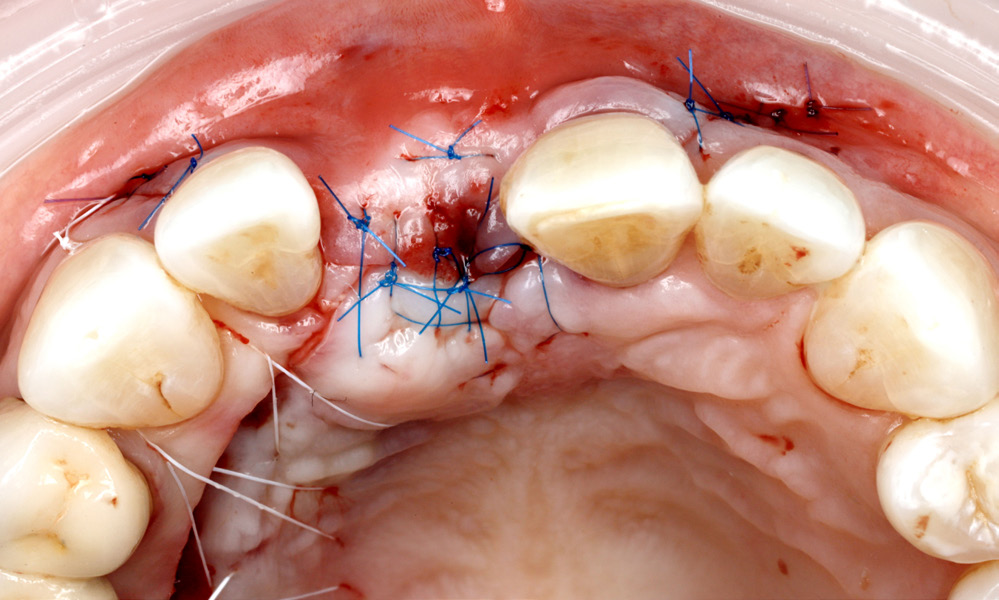
Procedure: A double graft technique was applied using a tuberosity graft at the level of the implant platform (Figure 3) and VIP-CTG over the top of the tuberosity graft stabilized to the split-thickness bed created during the split-thickness flap design (Figure 4). The tuberosity graft and VIP-CTG both need to be stabilized independently to the periosteum to remain immobile during healing (Figure 3, 4), 6.0 chromic gut or 6.0 glycolon sutures can be utilized.



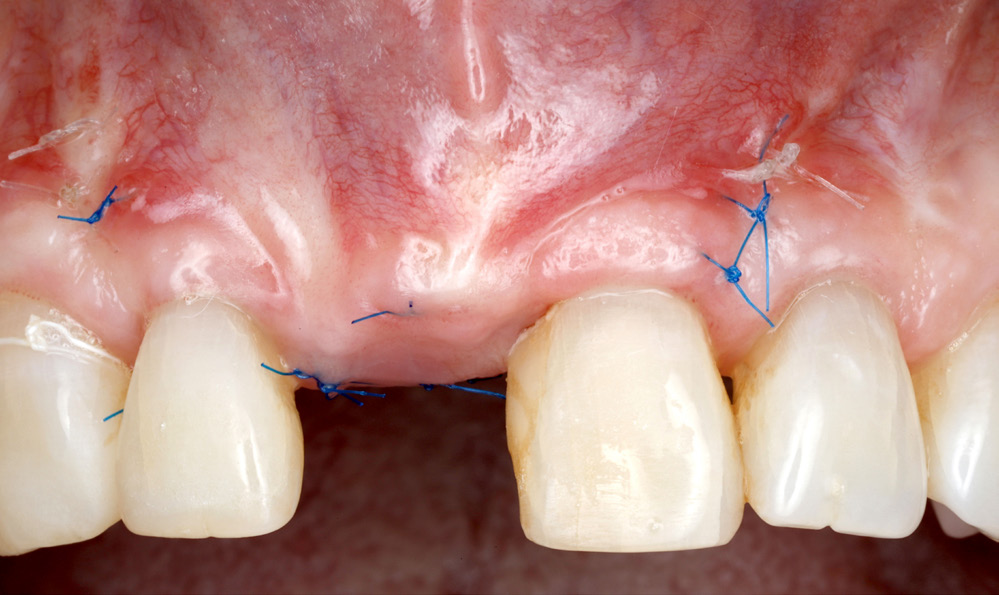
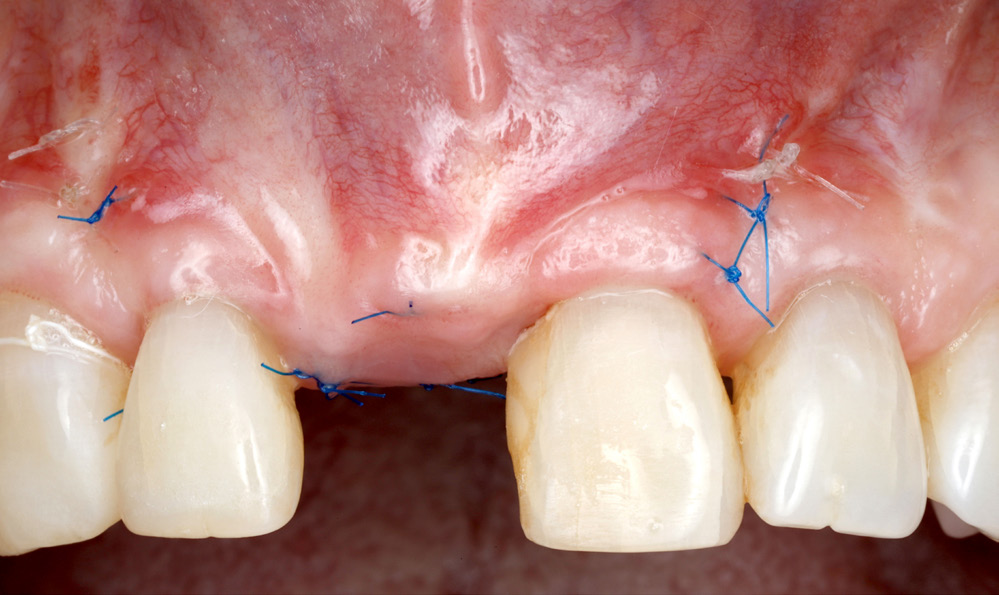
A sound primary closure over the grafted sites is accomplished thru a passive tissue release internally (Figure 5) using simple interrupted 6.0 proline sutures, while the palate can be closed using mattress PTFE sutures. Notice, the flap was advanced coronally over the exposed root at #10. All sutures can be removed after 2 weeks of healing. 2 months post-op healing, showing a significant gain in soft tissue volume and stable root coverage at #10 (Figure 6).
CASE 2
Augmentation Of Midline Papilla Height In Conjunction With Implant Placement At #8

A 52-year-old female referred for implant placement at site #8, clinically missing the midline papilla due to several failed attempts to place an implant by another dentist.
Implant placement and simultaneous ridge augmentation were completed 6 months prior to the soft tissue augmen- tation. The VIP CTG preparation starts with a split thickness flap to maintain all the soft tissue on the bed. This allows for the best blood supply, as well as the ability to suture the graft to the bed.


Harvest and maintain the graft attached to the incisive canal vasculature to maintain its blood supply (Figure 1), keeping the graft as thick as the palate will allow is very important for maximizing the CT gains. Note the thickness of the remaining palatal flap tissue after harvesting was completed. The CT split must be anterior enough to allow sufficient mobilization of the graft buccally and anteriorly.


The split thickness design of the bed is visible in this Figure 3.
The VIP-CTG is repositioned and stabilized around the root of #9, making sure to have enough volume against the mesial surface of root #9. Internal stabilizing glycol on
6.0 sutures was used to compress the graft against the bed and against the root of #9 mesially (Figure 4).

The flap is advanced in a tension-free fashion and closed using 6.0 proline sutures. The palatal harvest site is closed using mattress PTFE sutures (Figure 5a, b).




4 weeks and 8 weeks post-op follow-up showing an adequate soft tissue thickness and height of the midline papilla. The probings at tooth root #9 are 1-2mm (Figure 6a, b, c).
After 2 months of tissue maturation, a chairside provisional was fabricated using a temporary abutment (Figure 7).


At 1 month post temporization, the midline papilla max- imized its potential height and the patient was sent to a restorative dentist for the final restoration of #7-9 to achieve the most esthetic results possible (Figure 8a, b).
CASE 3
Use Of Vip-ctg To Augment Sites Of Congenitally Missing Lateral Incisors In Young Patient Unsuited For Implant Placement


A 17-year-old male patient was referred for soft tissue augmentation at sites #7 and 10 prior to placement of bonded Maryland bridges until the patient is ready for implant placement. VIP-CTG is planned at sites #7 and 10 to give the sites the maximum volume of soft tissue until the patient turns at least 20-21 years of age.


Step 1: create a donor site with the thickest possible pedicle CTG (Figure 2).
Harvesting a split-thickness VIP-CTG requires taking the connective tissue all the way thru the periosteum. Buccally, a full-thickness tunnel was created at both edentulous sites #7 and 10. The VIP CTG was stabilized in the buccal tunnel, and the flap was advanced and closed tension-free.



3 months follow-up after augmentation, the patient was sent back to the referral dentist for Maryland bridge restorations and tissue conditioning.
Final Thoughts
Soft tissue management procedures in today’s era of implantology play a paramount role in restorative and surgical implant dentistry. The presence of an adequate zone of keratinized tissue and adequate connective tissue thickness are both needed for peri-implant bone maintenance and the most esthetic results. Autogenous connective tissue grafts have been the gold standard for gaining an adequate tissue thickness around teeth and dental implants. Free connective tissue grafts can only provide a limited thickness gain due to the loss of vascularity and size of the harvested grafts, whereas the use of Vascularized Interpositional Connective tissue grafts (VIP-CTG), also known as pedicle grafts, can maximize the thickness gains and the ability to build tissue horizontally and vertically with longer term stability.
Reference
- Tseng ES, Tavelli L, Wang HL. Palatal pedicle flaps for soft tissue augmentation. The International Journal of Periodontics & Restorative Dentistry. 2020;40(4):581-588
- Sclar A, editor. Vascularized interpositional periosteal-connective tissue flap. In: Soft Tissue and Esthetic Considerations in Implant Dentistry. Chicago: Quintessence Publishing; 2003. p. 163.
- Levine, R.A., Martin, W. “Esthetic Risk Assessment in Implant Dentistry,” Inside Dentistry. 2012.
- Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: A systematic review. Journal of Dental Research. 2012;91(3):242-248
- Sclar AG. Soft Tissue and Esthetic Considerations in Implant Therapy. Carol Stream, IL: Quintessence; 2003

VIP-CTG is the last resort
ABSTRACT
The esthetic zone is the most visible area of the mouth when you smile. Thus, implants in the esthetic zone pose the most challenge in cases with multiple implants or pre-existing soft tissue or hard tissue deficiencies. Given the many challenges in the esthetic zone, even the slightest deviation from the most ideal plan can lead to esthetic failure and ultimately patient dissatisfaction.
Soft tissue deficiencies are usually the main risk factor around dental implants, especially in the esthetic zone. A lack of soft tissue volume can present in many clinical situations, including attachment loss on adjacent teeth (gum recession), concavities at sites with congenitally missing teeth, and loss of interdental papillae. A significant loss of soft tissue volume can be acquired at various phases, including a loss of bone and tissue volume after tooth extractions, history of periodontal disease, history of endodontic failures or vertical root fractures, and biological implant complications.
The clinical management of these various situations may be very different, involving soft and hard tissue reconstruction with further tissue training during the temporization phase. The use of free autogenous connective tissue grafts is usually limited to smaller ridge defects due to limited donor site availability and post-operative shrinkage of the tissue (1). Pedicled autogenous grafts have been proposed to overcome the limited gain of soft tissue volume when using palatal tissue (2,3).
My article describes how to augment and correct soft tissue deficiencies in the esthetic zone using a Vascularized Interpositional Periosteal-Connective Tissue Graft (VIP-CTG) in 3 clinical situations:
- esthetic management in the case of a poorly placed implant,
- soft tissue augmentation in the case of a severe vertical and horizontal deficiency, and (3) site management in the case of congenitally missing incisors in a younger patient unsuited for dental implants due to their age.
INTRODUCTION
The periodontal and peri-implant soft tissue thickness and zone of keratinized gingiva all play an important role in a patient’s esthetic clinical appearance, the soft and hard tissue health around teeth, and more importantly dental implants, especially as we have moved away from a purely functional and survival-based implant success definition to more patient-oriented esthetically driven, natural in appearance tooth and implant restoration (4). Autogenous connective tissue grafts are still the gold standard for almost all soft tissue augmentation procedures. Connective tissue (CT) can be obtained via a free graft approach or pedicled graft approach. While free grafts are completely removed from the donor site and placed in a remote site, pedicle grafts remain attached to their blood supply and are placed immediately next to the blood supply origin (incisive vasculature or greater palatine vasculature). Retention of the blood supply has a direct positive effect on graft volume stability and less shrinkage over time. (5)
Case 1
Management Of Poorly Positioned Implant And Gingival Recession On Natural Tooth In Esthetic Zone



A 42-year-old female patient was referred for an esthetic evaluation of a recently placed and restored implant at #9 and recession on tooth #10. The implant was very buccally positioned (by another dentist), but the patient declined removal of the newly placed implant. The decision was made to augment the soft tissue esthetics at sites #9 and 10 using a VIP-CTG.
The implant restoration at #9 and composite on tooth #10 were removed, and a cover screw was placed 3-4 days prior to soft tissue augmentation to allow soft tissue closure over the implant. This leads to a better primary closure during the surgical phase of treatment (Figure 2).


Procedure: A double graft technique was applied using a tuberosity graft at the level of the implant platform (Figure 3) and VIP-CTG over the top of the tuberosity graft stabilized to the split-thickness bed created during the split-thickness flap design (Figure 4). The tuberosity graft and VIP-CTG both need to be stabilized independently to the periosteum to remain immobile during healing (Figure 3, 4), 6.0 chromic gut or 6.0 glycolon sutures can be utilized.



A sound primary closure over the grafted sites is accomplished thru a passive tissue release internally (Figure 5) using simple interrupted 6.0 proline sutures, while the palate can be closed using mattress PTFE sutures. Notice, the flap was advanced coronally over the exposed root at #10. All sutures can be removed after 2 weeks of healing. 2 months post-op healing, showing a significant gain in soft tissue volume and stable root coverage at #10 (Figure 6).
Case 2
Augmentation Of Midline Papilla Height In Conjunction With Implant Placement At #8

A 52-year-old female referred for implant placement at site #8, clinically missing the midline papilla due to several failed attempts to place an implant by another dentist.
Implant placement and simultaneous ridge augmentation were completed 6 months prior to the soft tissue augmen- tation. The VIP CTG preparation starts with a split thickness flap to maintain all the soft tissue on the bed. This allows for the best blood supply, as well as the ability to suture the graft to the bed.


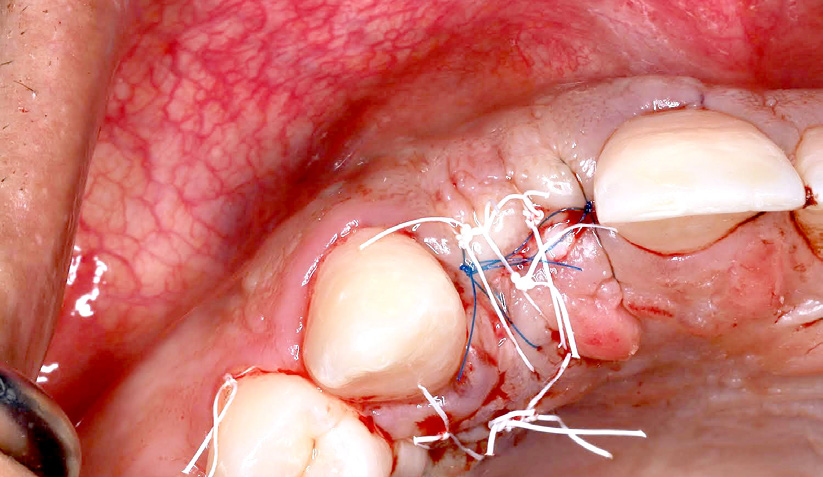
Harvest and maintain the graft attached to the incisive canal vasculature to maintain its blood supply (Figure 1), keeping the graft as thick as the palate will allow is very important for maximizing the CT gains. Note the thickness of the remaining palatal flap tissue after harvesting was completed. The CT split must be anterior enough to allow sufficient mobilization of the graft buccally and anteriorly.


The split thickness design of the bed is visible in this Figure 3.
The VIP-CTG is repositioned and stabilized around the root of #9, making sure to have enough volume against the mesial surface of root #9. Internal stabilizing glycol on
6.0 sutures was used to compress the graft against the bed and against the root of #9 mesially (Figure 4).

The flap is advanced in a tension-free fashion and closed using 6.0 proline sutures. The palatal harvest site is closed using mattress PTFE sutures (Figure 5a, b).




4 weeks and 8 weeks post-op follow-up showing an adequate soft tissue thickness and height of the midline papilla. The probings at tooth root #9 are 1-2mm (Figure 6a, b, c).
After 2 months of tissue maturation, a chairside provisional was fabricated using a temporary abutment (Figure 7).


At 1 month post temporization, the midline papilla max- imized its potential height and the patient was sent to a restorative dentist for the final restoration of #7-9 to achieve the most esthetic results possible (Figure 8a, b).
Case 3
Use Of Vip-ctg To Augment Sites Of Congenitally Missing Lateral Incisors In Young Patient Unsuited For Implant Placement


A 17-year-old male patient was referred for soft tissue augmentation at sites #7 and 10 prior to placement of bonded Maryland bridges until the patient is ready for implant placement. VIP-CTG is planned at sites #7 and 10 to give the sites the maximum volume of soft tissue until the patient turns at least 20-21 years of age.


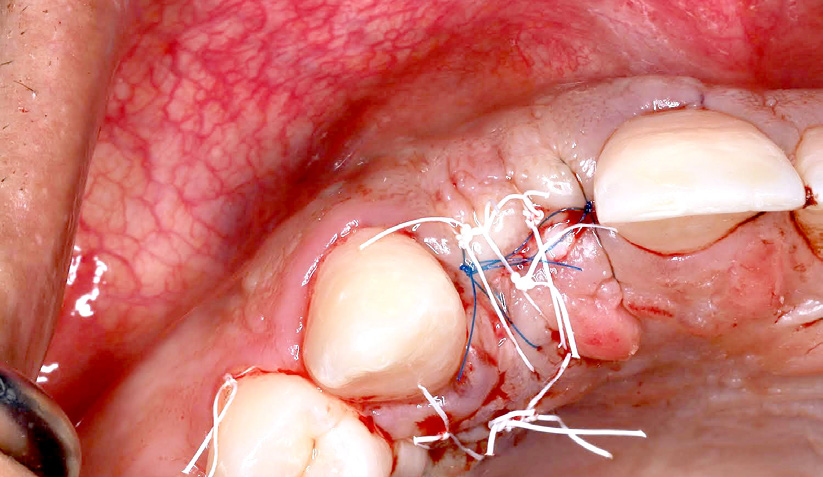
Step 1: create a donor site with the thickest possible pedicle CTG (Figure 2).
Harvesting a split-thickness VIP-CTG requires taking the connective tissue all the way thru the periosteum. Buccally, a full-thickness tunnel was created at both edentulous sites #7 and 10. The VIP CTG was stabilized in the buccal tunnel, and the flap was advanced and closed tension-free.



3 months follow-up after augmentation, the patient was sent back to the referral dentist for Maryland bridge restorations and tissue conditioning.
Final Thoughts
Soft tissue management procedures in today’s era of implantology play a paramount role in restorative and surgical implant dentistry. The presence of an adequate zone of keratinized tissue and adequate connective tissue thickness are both needed for peri-implant bone maintenance and the most esthetic results. Autogenous connective tissue grafts have been the gold standard for gaining an adequate tissue thickness around teeth and dental implants. Free connective tissue grafts can only provide a limited thickness gain due to the loss of vascularity and size of the harvested grafts, whereas the use of Vascularized Interpositional Connective tissue grafts (VIP-CTG), also known as pedicle grafts, can maximize the thickness gains and the ability to build tissue horizontally and vertically with longer term stability.
Referance
1.Tseng ES, Tavelli L, Wang HL. Palatal pedicle flaps for soft tissue augmentation. The International Journal of Periodontics & Restorative Dentistry. 2020;40(4):581-588
2.Sclar A, editor. Vascularized interpositional periosteal-connective tissue flap. In: Soft Tissue and Esthetic Considerations in Implant Dentistry. Chicago: Quintessence Publishing; 2003. p. 163.
3.Levine, R.A., Martin, W. “Esthetic Risk Assessment in Implant Dentistry,” Inside Dentistry. 2012.
4.Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: A systematic review. Journal of Dental Research. 2012;91(3):242-248
5.Sclar AG. Soft Tissue and Esthetic Considerations in Implant Therapy. Carol Stream, IL: Quintessence; 2003

Contact
Dr. Dmitriy Ivanov, DDS
Board Certified Periodontist and Implant Specialist
Address: 16055 Ventura Blvd. Suite 405 Encino, CA 91436
Email: Dmitriyivanov.dds@gmail.com
Instagram: perioimplant_LA
Web: www.perioamigos.com
